There’s currently no defined time period or upper limit, yet many women are wrongly told that they can use HRT for a maximum of 5 years or until the age of natural menopause. This decision should be based on your own informed choice and be reviewed annually with your health care provider.
What is the difference between body identical and bioidentical HRT?
Body identical HRT describes licensed, regulated hormones – usually derived from the yam root vegetable – which are chemically identical to the hormones produced naturally by the body. These can be prescribed by NHS and private GPs or menopause specialists.
Bioidentical HRT is a marketing term for unlicensed, unregulated hormone preparations prescribed in some private clinics. These are not approved or recommended for use by the British Menopause Society (BMS).
What are the benefits and risks of HRT?
Taking HRT can relieve your menopause symptoms and help to protect your long-term bone health, reducing your risk of osteoporosis (thinning of the bones) and bone fracture.
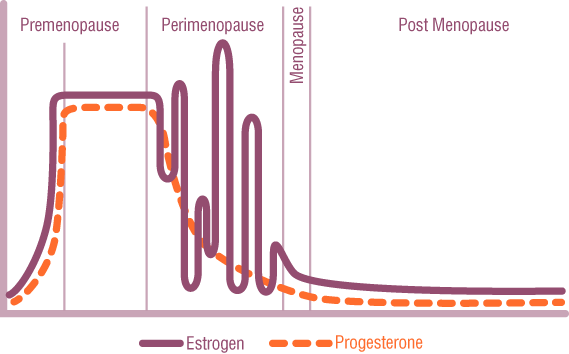
According to the Royal Osteoporosis Society, the lifetime risk of bone fracture for women over the age of 50 is about 1 in 2, compared to 1 in 5 for men. It’s important to consider this during perimenopause when oestrogen levels are falling.
Evidence suggests that starting HRT within 10 years of menopause under the age of 60 reduces the risk of cardiovascular disease. You can read more about this on the British Heart Foundation website – menopause and your heart.
The subject of HRT often raises concerns about breast cancer as a result of news headlines that appeared after the Women’s Health Initiative study was published in 2002. The long-term follow up from that study found that for most women the benefits of HRT outweigh the risks. You can read more about this on the British Menopause Society (BMS) website.
What is local oestrogen?
Local oestrogen is tiny doses of oestrogen hormone, applied directly to the vulva and vagina. It’s used to manage urinary, vaginal and vulval symptoms, including dryness, soreness, irritation, urinary urgency (a sudden need to pee), and repeated urinary tract infections.
Local oestrogen is available as creams, pessaries, gels, or a vaginal ring and is safe to take lifelong.
 HRT should be offered as the recommended first line treatment for symptoms related to perimenopause and menopause. HRT is designed to relieve the symptoms associated with oestrogen deficiency and is available as tablets, patches, gels and a spray all of which need to be prescribed at the right dose for individual women; there is absolutely no one size fits all.
HRT should be offered as the recommended first line treatment for symptoms related to perimenopause and menopause. HRT is designed to relieve the symptoms associated with oestrogen deficiency and is available as tablets, patches, gels and a spray all of which need to be prescribed at the right dose for individual women; there is absolutely no one size fits all.
